
For years, tendon pain was labelled tendinitis, a term suggesting inflammation (“-itis”). But advancements in research and imaging have completely reshaped how we understand tendon conditions, and with that shift comes a new (and more accurate) name: tendinopathy.
This isn’t just a terminology update… it’s a fundamental change in how we diagnose, understand and manage tendon pain.
Modern research has shown that most tendon pain does not involve inflammation at the tendon level. This discovery challenged the entire treatment approach, because the old model relied heavily on anti-inflammatories and rest. We now know that anti-inflammatory medication can actually have a negative impact on healing and that rest actually makes this condition worse!
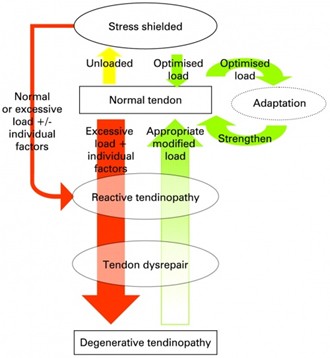
The updated understanding revealed something far more complex:
Because of this, the umbrella term tendinopathy is now used, accurately capturing the various stages a tendon can move through.
Tendons aren’t just passive ropes connecting muscle to bone.
They:
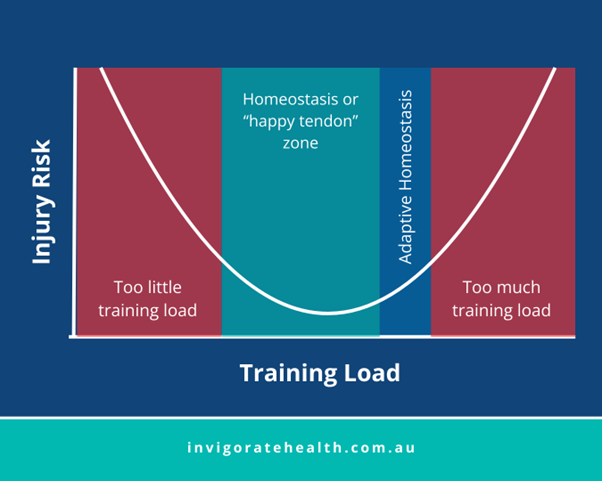
To do this effectively, tendons function best within a “happy zone”, a range of load where they operate efficiently and without pain.
When load suddenly increases (or decreases), tendons can exceed their zone of tolerance, leading to pain and dysfunction.
This is your tendon’s first warning sign.
It’s a short-term, non-inflammatory response to a sudden spike or drop in load.
What you’ll notice:
• pain after exercise
• tenderness that settles within hours
• intermittent symptoms
What’s happening inside the tendon:
• mild thickening
• temporary changes to protect from stress
Good news:
This stage is often reversible with load modification.
This happens when overload continues and the tendon can’t recover adequately.
What you’ll notice:
• more consistent pain
• flare-ups with activity
• less tolerance to load
Inside the tendon:
• disorganisation of collagen
• increased blood vessel and nerve growth
• early structural change
With proper management, this stage can still be reversed.
This is the most advanced stage, often seen in older adults or people with long-term tendon pain.
What you’ll notice:
• fluctuating pain
• stiffness
• reduced capacity
Inside the tendon:
• cell death
• structural breakdown
• reduced mechanical strength
Although structural changes may not fully reverse, symptoms can still improve dramatically with the right plan.
No matter which tendon is affected, achilles, patellar, gluteal, elbow, rotator cuff, the treatment principles are similar.
Our evidence-based approach includes:
Progressive Loading Program:
This strengthens the tendon, restores function, and increases load tolerance.
Optimising Training Load:
We help you adjust volume, frequency, and intensity to keep your tendon in its “happy zone.”
Correcting Strength and Mobility Deficits:
Weak or tight surrounding muscles often contribute to tendon stress.
Education:
Understanding your condition helps you rehab confidently and avoid recurrence.
Early intervention means fewer structural changes and better outcomes. In saying that, even in degenerative tendinopathy, improvement is absolutely possible with the right program.
Whether your tendon is freshly irritated or has been bothering you for years, our Physios and Chiros can help guide you through a targeted, evidence-based rehab program.
(Published Jan 2, 2026)
Written by: Anouska Symons (Senior physiotherapist)